"Early detection saves lives. Don’t be afraid to check yourself." – Movember Foundation
It is highly recommended that you monitor yourself for any uncommon symptoms for an early detection of testicular cancer. Fortunately, the good part is that testicular cancer is rare and it affects around 1 among 100,000 men in India. This blog will help you understand everything about testicular cancer prevalence in India, its awareness, survival rates, etc.
Introduction to Testicular Cancer
 Testicular cancer the name itself suggests that it arises in the testicles, which are found within the scrotum, a loose bag of skin under the penis. The testicles produce male sex hormones and sperm for reproduction As mentioned above compared to other cancers, testicular cancer is relatively rare. And is more common in white men than in Asian or African men. In India, it is rare, affecting fewer than 1 in 100,000 men. It is the most common cancer in 20- to 35-year-old men.
Testicular cancer the name itself suggests that it arises in the testicles, which are found within the scrotum, a loose bag of skin under the penis. The testicles produce male sex hormones and sperm for reproduction As mentioned above compared to other cancers, testicular cancer is relatively rare. And is more common in white men than in Asian or African men. In India, it is rare, affecting fewer than 1 in 100,000 men. It is the most common cancer in 20- to 35-year-old men.
Testicular Cancer in India: An Overview
As per NIH testicular cancer is the most common cancer found in young men aged 15 to 40. It makes up 1% of all cancers in adults and 5% of urological cancers. Western countries see between 3 and 11 new cases per 100,000 men annually.
Noticing particularly in India testicular cancer occurs in 0.3% of all cancers and is in 31st place among all types of cancers.
Testicular Cancer Cases by Region (2020)
Region |
Total Cases |
Incidence Rate (per 100,000 men) |
Key Insights |
|
Global |
74,458 |
Varies by region |
Most common in young men (15–40 years); survival rate 95% (all stages), 99.2% (localized). |
|
North America |
10,617 |
5.9 |
White men: 8.3, Hispanic men: 4.6, Black men: 1.5; 460 deaths projected in 2022. |
|
South America & Caribbean |
13,653 |
Varies by country |
Brazil (3,388 cases), Mexico (3,337), and Argentina (2,047); have the highest rates in Argentina (8.7), Uruguay (8.1), and Chile (7.6). |
|
Europe |
25,058 |
Western: 8.7, Northern: 7.2, Southern & Central: 5.9, Eastern: 3.2 |
Highest global incidence; Norway (11.8), Slovenia (10.8), Denmark (10.4). |
|
Africa |
3,302 |
0.3–0.6 |
Lowest incidence globally; likely underreported due to healthcare limitations. |
|
Asia & Middle East |
20,651 |
Varies by country |
India (4,638 cases, 0.46 rate), China (4,502, 1.6), Japan (2,458, 2.9), Turkey (1,605, 4.0). |
Is Testicular Cancer Common in India?
Thankfully testicular cancer is not so common in India this is for the reason that it affects under 1 in 100,000 men. Along with India, it is least common in a few other parts of the world such as Asian and African countries as well.
Also, read - Is India becoming the Cancer capital of the world?
Testicular Cancer Survival Rate in India
The survival rate of testicular cancer In India depends on many factors such as early detection, treatment access, and the stage of cancer the person is dealing with. So it is estimated to be around 85-90% relying on those mentioned factors.
How Testicular Cancer Occurs
 While the exact cause of testicular cancer remains unknown you can look into a few risk factors that may increase the likelihood of developing cancer. These include:
While the exact cause of testicular cancer remains unknown you can look into a few risk factors that may increase the likelihood of developing cancer. These include:
1. Undescended Testicle (Cryptorchidism)
The first cause that stands out as the first reason for the occurrence of testicular cancer is undescended testicle a condition where Infants born with one or both testicles fail to move into the scrotum and have a higher risk of testicular cancer, even if surgery is performed later.
2. Family History
Genetics can be an additional reason that serves as the likelihood of developing testicular cancer so having a close relative with testicular cancer increases the risk for you to have the testicular cancer.
3. Personal History of Testicular Cancer
Some cases reported that if you've had testicular cancer in one testicle, the chances of developing it in the other are significantly higher.
4. Infertility
Some studies suggest that infertility may be linked to a higher risk of testicular cancer, possibly due to underlying genetic or hormonal factors.
5. HIV and AIDS
Men with HIV/AIDS, especially those with low immune function, are at a greater risk of cancer.
6. Physical Features (Hypospadias)
Individuals born with hypospadias, a condition where the urethra opens on the underside of the penis, may have an increased risk.
7. Cannabis Use
As per research, regular cannabis use might contribute to a higher risk of developing testicular cancer, though further studies are needed for the same.
8. Intersex Variations
People with certain intersex conditions, such as partial androgen insensitivity syndrome, may have an increased risk of developing testicular cancer.
What Does NOT Cause Testicular Cancer?
There is no particular evidence that the following conditions may develop testicular cancer:
❌ Injury to the testicles
❌ Sporting strains
❌ Hot baths or saunas
❌ Wearing tight underwear
Symptoms of Testicular Cancer
 Generally, testicular cancer often presents with mild symptoms in the early stages, making self-examinations and early detection are highly recommended by uro-oncologists. Here are a few common symptoms to watch out for:
Generally, testicular cancer often presents with mild symptoms in the early stages, making self-examinations and early detection are highly recommended by uro-oncologists. Here are a few common symptoms to watch out for:
Lump or Swelling in the Testicle
A painless lump or swelling in one testicle is the most common symptom. May feel like a hard or irregular mass around there.
Testicular Pain or Discomfort
There are a few cases where a few people may experience dull aching or discomfort in the affected testicle or scrotum. Sharp pain is less common but there are chances that it can occur.
Heaviness in the Scrotum
A sensation of weight or fullness in the lower abdomen or scrotum is also a symptom of testicular cancer.
Changes in Testicle Size or Shape
For people diagnosed with testicular cancer, one of their testicles becomes larger or firmer than usual. Also, due to the buildup of fluid in the scrotum which condition called hydrocele can cause a noticeable swelling of the testicle.
Lower Abdominal or Groin Pain
When you experience persistent pain or discomfort in the lower abdomen, groin, or back can be a notification to indicate that cancer is spread to other areas in the body.
Breast Enlargement or Tenderness (Gynecomastia)
In rare cases, hormonal imbalances caused by cancer can lead to breast swelling or tenderness as well.
Back Pain or Shortness of Breath (Advanced Cases)
If cancer spreads to lymph nodes or lungs, it may cause:
You might experience back pain (from lymph node involvement) in advanced conditions when the cancer is spread.
Also, shortness of breath, coughing, or chest pain can come across (if cancer reaches the lungs).
How Testicular Cancer is Diagnosed
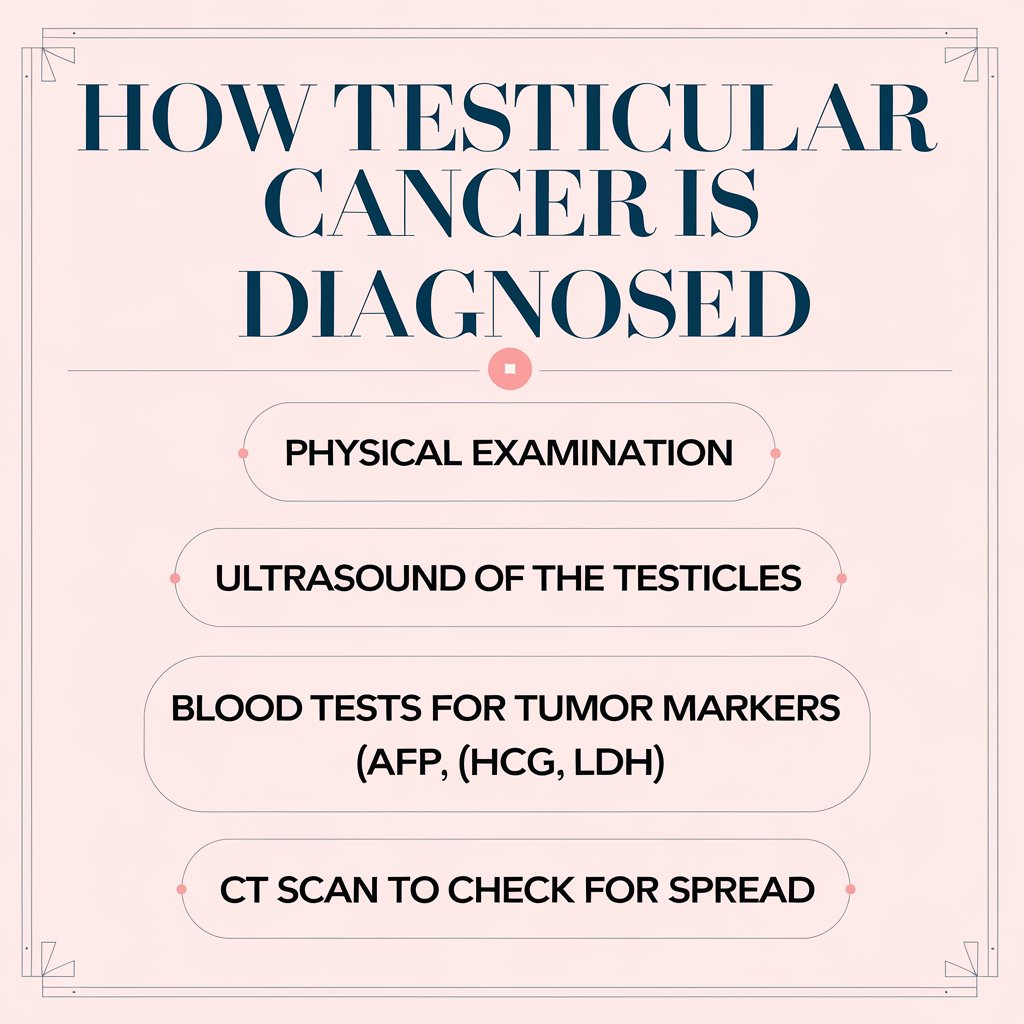 If you notice any changes in your testicles, the earlier the better the treatment. You will be allocated for the following tests to diagnose testicular cancer.
If you notice any changes in your testicles, the earlier the better the treatment. You will be allocated for the following tests to diagnose testicular cancer.
Physical Examination – This is performed so the doctor checks for lumps, swelling, or any testicle abnormalities.
Ultrasound – It helps confirm the presence of a tumor or abnormal mass in the testicle.
Blood Tests (Tumor Markers) – Measures levels of:
Alpha-fetoprotein (AFP)
Beta-human chorionic gonadotropin (β-hCG)
Lactate dehydrogenase (LDH)
Surgical Removal (Inguinal Orchiectomy) – The only way to confirm testicular cancer. The entire testicle is removed through an incision in the groin.
A biopsy is NOT done (cutting into the testicle may spread cancer cells).
CT Scan (Chest and abdomen): This was done to check if the cancer has spread to other parts of the body.
Treatment Options for Testicular Cancer
 After diagnosing testicular cancer the treatment procedure may vary depending on factors such as seminoma or non-seminoma, stage, and overall health of the patient. Here are the primary treatment approaches:
After diagnosing testicular cancer the treatment procedure may vary depending on factors such as seminoma or non-seminoma, stage, and overall health of the patient. Here are the primary treatment approaches:
Surgery:
The first line of treatment for testicular cancer is surgery, which removes the testicle, and the process called high inguinal orchidectomy a procedure where the affected testicle is removed through an incision in the groin. Performing this surgery not only eliminates the primary tumor but also helps in diagnosing the cancer type as well.
Retroperitoneal Lymph Node Dissection:
The process of removing lymph nodes is called Retroperitoneal Lymph Node Dissection - RPLND. This is done as the cancerous cells get spread to the retroperitoneal lymph nodes which are located near major blood vessels at the inferior vena cava and aorta. In non-seminoma cancers,, commonly, these nodes remain enlarged after chemotherapy so RPLND is performed. One of the treatment procedure is that robotic-assisted RPLND.
Chemotherapy
Chemotherapy is performed in most of the cancers to destroy those cancer cells and it uses cytotoxic drugs to kill cancer cells throughout the body. So if you are diagnosed with testicular cancer chemotherapy is recommended in cases where the cancer has spread beyond the testicle, especially to lymph nodes, adjuvant chemotherapy is when there is a risk of recurrence after surgery and when the cancer has returned after initial treatment.
You might also experience a few side effects after undergoing chemotherapy such as nausea, loss of appetite, fatigue, weakened immune system, weight loss, easy bruising, or bleeding.
Radiotherapy
If you are someone diagnosed with seminoma type of testicular cancer radiotherapy would be effective. So it involves directing high-energy X-rays at the retroperitoneal lymph nodes to destroy cancer cells. Also, radiotherapy is usually given in short daily sessions over 3 to 4 weeks.
Read more on Urological Concerns.
The bottom line:
Awareness and early detection are key to saving lives with a higher cure rate than any cancer testicular cancer treatment is highly effective. So, if you are someone experiencing any unusual symptoms such as lumps, pain or swelling in the testicles do visit a urologist immediately.

